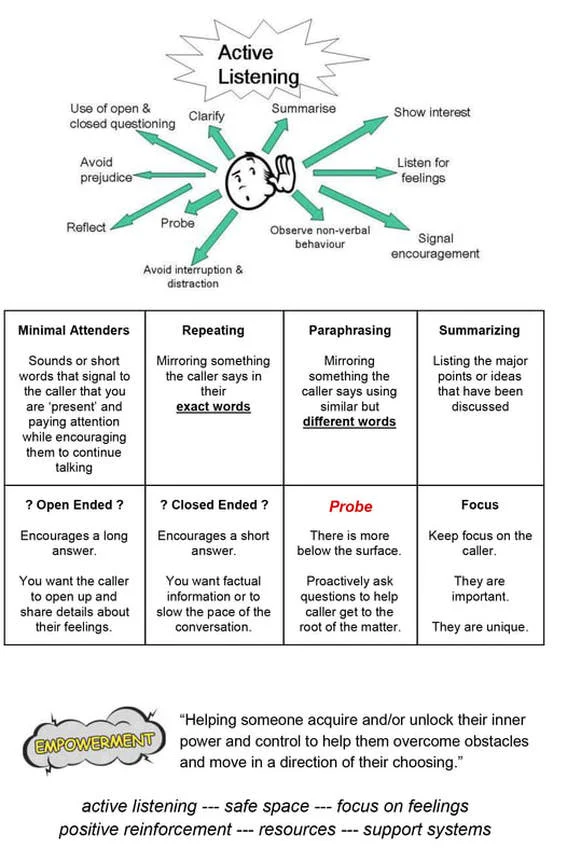
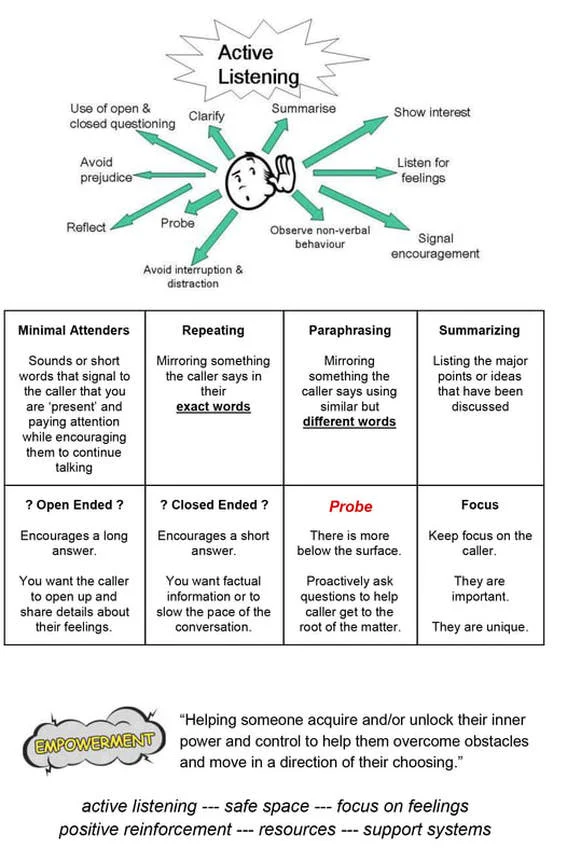
Active Listening
First, we can answer questions about gay, lesbian, bisexual or transgender issues.
Second, we maintain information on local resources for cities and towns across the United States. (Also Canada and internationally)
And Third, we provide peer-support if someone is going through a difficult time, and just needs to chat for a few minutes. How can I help you?
Coming out (of the closet) can mean a lot of things; it’s different for each person. Generally, it can mean, acknowledging that a person is LGBT.
Coming out can mean (but not limited to):
coming out to classmates / workmates
coming out to close friends
coming out to siblings or cousins or other family members
coming out to parents or guardians
coming out to everyone you know all at one
coming out the select people you choose and trust
coming out to yourself and feeling good about who you are.
A coming out journey is personal and no two are alike.
There is no wrong way or only one right way of coming out, there is only what makes the most sense to the caller.
A person’s coming out process can change as they grow and become more comfortable with themselves.
The decision to come out to another person can be the caller’s decision. They can consider the pros and cons of coming and what it means specifically for them.
We’re sorry if someone has outed them without their consent.
If minors: they may need to decide if they want to come out now, or wait until they are more independent. It may not be safe for them to come out to family members and their safety is very important. They may decide that their parents have not earned the right to know this about them yet. Not coming out to any specific person does not invalidate who they are, they get to choose when and who they want to come out to on their own terms.
There are no right or wrong answers; just what makes the most sense to the caller.
Being Born Lesbian, Gay, Bisexual …
It might be helpful to know that just about all mainstream experts on human sexuality believe that someone’s sexual orientation, regardless of whether it’s gay, straight, bi, or pan, is something that forms in a person’s life before they are born, or within the first few years of a person’s life.
Sexual orientation forms way before a person is making conscious decisions about anything. To being Lesbian, Gay, Bi or Pan may not be as common as being straight, but they are definitely considered just as normal.
No one chooses their sexuality, it is just part of who they are. It is a normal and natural part of who they are.
How do you know
When someone is trying to understand their sexual orientation is, it can help to focus on long-term feelings and attractions, rather than on events that might have happened.
So if a person is trying to figure things out, it can help to think about how long they have had feelings
for people of the same gender (or people beyond just the same gender)
how strong those feelings are
Being born Transgender
It might help to know that just about all mainstream experts on gender identity believe that a person’s gender identity regardless of being transgender or cisgender is something that forms in each person before we are born or in the first few years of a person’s life, long before any conscious decisions are made. While being transgender, genderqueer, non-binary, etc may not be as common as identifying as cisgender, they are all considered just as normal.
No one chooses their gender, it is just part of who they are. It is a normal and natural part of who they are.
How do you know
When someone is trying to understand their gender identity, it can help to focus on long-term feelings and how they feel about their identity NOT what other people may say or believe.
do you feel comfortable being referred to as a boy/man or girl/woman
how do you feel in your body. Does the outside of your body line up with how you feel on the inside?
Has the development of sex characteristics (breast, facial, body hair, etc) during puberty cause an uncomfortable feeling or traumatic experience. (Dysphoria) Do they cause body image issues?
Lots of STD’s – WE FOCUS ON HIV/AIDS
When we talk about safer-sex information here, we are focusing specifically on HIV risk, since that’s the most serious type of sexually transmitted infection (STI), but it isn’t the only one. So this information is just about HIV transmission.
If callers/chatters have questions on other STIs or more detailed information on sexual activities they can contact the
Sex, Gender and Relationship Hotline, 415-989-7374, wwwsgrhotline.org (Formerly the San Francisco Sex Information Switchboard).
General Overview
The way that HIV can transmit is by getting certain very specific fluids from one person’s body directly into another person.
The fluids that you have to be most concerned with are blood, semen (cum), maybe pre-cum, and vaginal fluids.
Always Assume HIV+ when with a partner
If you’re going to be with anyone, the safest thing to do is assume that it’s possible that the person you are with might have been exposed to HIV at some point in their past, and protect yourself based on that possibility. That way you won’t have to guess about the other person.
Receiving Oral Sex: NO MEANINGFUL RISK
If someone is receiving oral sex, then they are just coming in contact with the other person’s mouth, and we know that saliva does not transmit HIV. We have never seen any cases of anyone getting HIV by receiving oral sex.
Performing oral sex on someone with a vagina: NO MEANINGFUL RISK
It is considered a theoretical risk to transmit HIV through oral contact with a vagina, due to possibly getting blood into the mouth. However, in the real world, we don’t really see it happening. If you want to reduce whatever risk might be there, you can use a latex barrier between the vagina and the other person’s mouth so that the fluids don’t get inside. Barriers that you can use would be a dental dam or you can cut open a latex condom or latex glove.
Performing oral sex on someone with a penis and only getting pre-cum in the mouth: VERY LOW RISK
It is important not to get A person’s semen (cum) into the mouth. One way is to talk with the person beforehand and let them know that you don’t want them to cum into your mouth.
If you can trust them on that, then the only possible risk is maybe from getting pre-cum in your mouth, and the likelihood of getting HIV just from pre-cum is very low. We are not aware of it ever happening. If you want to be even safer than that, you can have someone wear a condom when you’re performing oral sex on them.
Performing oral sex on someone with a penis and getting semen (cum) in the mouth: MEDIUM RISK
Getting semen (or cum) into the mouth, whether it is spit-out or swallowed, is considered a medium risk, and while it is not easy, we have seen people contract HIV by doing this. If you want to reduce that risk, you can have someone wear a condom when performing oral sex, or don’t have them cum directly into the mouth.
Anal sex or vaginal sex : HIGH RISK
This is considered to be the riskiest ways of transmitting HIV sexually, and the risk is high for both partners, although the risk is greater for the person being penetrated. It is really important to use a condom every single time. Not everyone has anal sex, so you will need to decide if it's something that you want to do.
If it is, then using a condom is really important. There are three things to remember about condoms:
1. Always use a new package of condoms, so check the expiration date on the wrapper (because condoms can expire or be exposed to wear and tear over time which can make them ineffective at preventing HIV).
2. Make sure the condom is made of latex (If someone is allergic to latex, they can use a a condom made of polyurethane instead).
3. Always use a water-based lubricant (because other types of lubricants can weaken and break latex condoms and make them ineffective at preventing HIV).
If you do these things, then you will substantially reduce the risk of transmitting HIV, but it won't eliminate the risk completely. But it will make it much safer than using no protection at all. In addition to condoms, there is now an option called PrEP, which is a prescription medication that must be taken on a specific schedule. When taken properly it is highly effective against infection with HIV. However, it does not protect people from other STI's (sexually transmitted infections), so it should be used along with condoms.
Kissing: NO MEANINGFUL RISK
HIV cannot be transmitted through saliva. This means that you cannot get HIV by only kissing someone. The only exception is if there are significant wounds, and the other person is bleeding into those wounds. From a practical standpoint, we don’t see that happening.
Sex between HIV-negative partners: NO RISK
You cannot get HIV by being sexually active in any way with someone who is HIV-negative. However, you should always assume that your partner(s) may have been exposed to HIV at some point in the past, and protect yourself based on that possibility. There is no way to know for sure if someone is HIV+ at the moment you are having sex with them. However, if you knew for a scientific fact that neither partner was exposed to HIV, then you cannot create HIV between you.
HIV risk for no-contact sexual behaviors: NO RISK
There is no risk of HIV for behaviors such as masturbation or other sexual activities which do not involve contact with another person, because there is no transfer of bodily fluids.
HIV risk simply for being LGBTQ: NO RISK
There is no inherent risk of HIV for simply being LGBTQ. There are misconceptions (primarily as a result of the AIDS epidemic in the 1980s) that have made some people believe that you will get HIV/AIDS no matter what, if you are LGBTQ. That is not true. Non-LGBT people can also become infected with HIV. What determines someone’s risk is what they do, not who they are.
Sex Toys & HIV Risk:
There is risk if you share them and don’t clean them between partners. This could happen because sex toys can sometimes cause cuts or tears inside one’s body, and if you are sharing toys and don’t properly clean them between partners, it can cause blood, semen, pre-cum or vaginal fluids to travel from one person’s body to the other, via the sex toy. To be as safe as possible when using a sex toy, don’t share your toys! If you must, use clean, disinfected toys only, and do not immediately share the toy between partners. If you do share, be sure to clean the toy thoroughly between each partner's use. You may also use a new, latex condom over a sex toy to reduce your risk of HIV.
PrEP (Pre-Exposure Prophylaxis)—taken before exposure
PREP is a prescription medication that must be taken on a specific schedule. When taken properly it is highly effective against infection with HIV. However, it does not protect people from other STI's (sexually transmitted infections), so it should be used along with condoms.
When taken properly, it is highly effective against getting infected with HIV. But it does NOT protect people from other STI’s (sexually transmitted infections) or pregnancy, so it should be used along with condoms. When someone first starts taking PrEP, it can take about seven days before it builds up enough in your system to be effective in preventing HIV infection. The long-term effects of taking PrEP are not yet known. NOTE: We do not have specific insurance/pricing information. If a caller is interested in PrEP, they can speak to their doctor (if comfortable), or an HIV clinic (find in database).
PEP (Post-Exposure Prophylaxis)—taken after exposure
If you have been exposed to HIV within the past 72 hours (3 days), you should seek medical attention (like urgent care or your doctor) ASAP to determine if PEP can be used to lower the risk of becoming infected with HIV, but it is not 100% effective. PEP is not an option after 72 hours.
PEP should only be used for emergency situations, and the sooner it is started within the 72 hour window, the better. Once prescribed, PEP is taken once or twice a day for 28 days. NOTE: We do not have specific insurance/pricing information. If a caller is interested in PEP, they can speak to their doctor (if comfortable), urgent care, or an HIV clinic (find in database).
Barriers
Condoms:
There are three things to remember about condoms:
1. Always use a new package of condoms, so check the expiration date on the wrapper (because condoms can expire or be exposed to wear and tear over time which can make them ineffective at preventing HIV).
2. Make sure the condom is made of latex (If someone is allergic to latex, they can use a a condom made of polyurethane instead).
3. Always use a water-based lubricant (because other types of lubricants can weaken and break latex condoms and make them ineffective at preventing HIV).
If you do these things, then you will substantially reduce the risk of transmitting HIV, but it won't eliminate the risk completely. But it will make it much safer than using no protection at all. For oral sex on a vagina, you may use a latex condom which has been cut open, if dental dams are unavailable.
Dental dams:
Dental dams are a thin sheet of latex which are an effective barrier against HIV when used while performing oral sex on someone with a vagina.
Internal/female condoms:
More research has to be done to be conclusive about whether internal/female condoms are effective enough in preventing HIV infection in vaginal or anal sex. For this reason, we currently do not recommend their use over regular latex condoms.
Latex gloves:
Latex gloves are not an effective barrier against HIV infection.
HIV Testing
Testing Fast Facts:
There is a “window period” for testing, which means that it takes up to 3 months before someone can get an accurate result on an HIV test. So, test results don’t count for anything that happened in the 3 months before the person was tested.
The HIV tests that we recommend are HIV-antibody tests. These involve a quick finger prick for a blood test (which is nearly painless) or a cheek swab.
It is important to get your testing done by a medical professional either at a doctor’s office or clinic because you’ll have immediate support, answers to any questions you may have, and a reliable result. So while there are at-home tests which can be highly accurate, being tested by medical professionals is the best option.
The results for an HIV test take about 20 minutes. NOTE: If in Canada, blood tests done by a medical professional are the only option in most provinces, and can take up to two weeks to process results. The window period is often shorter than 3 months for this type of test, so we recommend talking to a medical professional to know when to get tested.
Get tested regularly (every 3 to 6 months if having medium-to-high risk sex).
HIV FAQ:
I got a negative HIV test result! What now?
It’s great news to get a negative HIV test result, however it is important to not start putting yourself at risk because of it.
I got a positive HIV test result. What now?
PEER SUPPORT
My partner told me they are HIV negative/I know my partner is HIV negative:
We suggest that you are as safe as possible each time you are sexually active, even if you’re with the same person on a regular basis.
We cannot confirm someone else’s status, and so it is always safest to assume that your partner(s) have been exposed to HIV at some point in the past, and to practice safe sex consistently.
I don’t want to practice safe sex.
As long as there is consent between everyone involved, ultimately, it is up to you and your partner(s) what you engage in sexually, and whether you practice safe sex. If you’re interested in HIV information, we’re happy to offer that, but it’s up to you whether you choose to use it.
I am sexually active with someone other than my partner, and I do not want to tell them.
Consent and safety are our priorities at this organization, so I’d like to make sure you know that there are health risks for your partner and potential legal risks for you for endangering your partner’s health.
GENDER IDENTITY & EXPRESSION
It is very important to use the pronouns and gender terms the callers/chatters use for themselves.
These are just a few of the most often used pronouns. Others are just as valid. It is also valid to be questioning, not sure or not use one pronoun or label.
General Overview
The term “gender identity & expression” is an umbrella term that includes anything to do with gender and how a person chooses to express their gender identity.
Common terms to know (MORE TERMS CAN BE FOUND IN THE GLOSSARY)
Cisgender: Also abbreviated as Cis. Someone whose gender identity conforms to the sex assigned to them at birth. “cis” is Latin for “to remain on the same side of”.
Cross-dressing (replaced outdated term, transvestite): Cross-dressers may enjoy wearing the clothes of a gender they do not identify as. They may enjoy wearing the clothing of another gender, but do not identify as that gender. Cross-dressing does not imply anything about a person’s sexuality.
Gender Dysphoria: Emotional difficulty, depression and/or distress that can be caused by a person’s body, or how others interact with them or misgender them.
Gender Expression: How one expresses their gender, be it through clothing, makeup, hair, etc.
Gender-Fluid: An individual who may frequently change their gender expression and presentation.
Gender Identity: An individual’s internal sense of what their gender is, be it male, female or outside the binary. It may or may not align with their gender assigned at birth.
Gender Nonconforming/Gender Variant: Individuals who do not conform to society’s expectations of gender role.
Gender Queer: An individual who may not subscribe to society’s expectations of gender distinctions but identifies with neither, both, or some combination of male and female genders.
Non-Binary / NB: Individuals who do not identify as either male or female, but rather outside the gender binary. The term can be used both as a self-identifier, but also to encompass any other identities that do not fit into the binary gender. Non-binary people may or may not identify as trans.
Questioning: An individual who may be trying to understand or questioning their sexuality and/or gender identity.
Transgender: Individual whose gender identity differs from the sex assigned to them at birth.
Transsexual: Similar to Transgender, this is a more specific term typically referring to trans people who are hormonally and/or surgically transitioning from one binary gender to another. This term has largely fallen out of use. This term is fairly out of use among younger trans people and should be avoided unless the individual self-identifies.
Transitioning: Transitioning is the word used to describe the process that a transgender person goes through when they want to change their appearance from the way they look externally, to the correct gender they know they really are. How someone chooses to transition can vary greatly from one person to another. Some people transition by changing the clothes that they wear, or the way they wear their hair, or by using (or not using) makeup. Other people might choose to make more physical changes to their appearance by working with a knowledgeable doctor for hormone treatments. Depending on the individual, hormones can change the texture of the skin, can alter where and how hair grows and can sometimes change the pitch of someone’s voice. And then a very small percentage of people might choose to have sex-reassignment surgery. This is not done often because of the significant cost involved. The actual surgery can also vary depending on whether someone wants “top” (of the body) surgery or “bottom” or both.
Acceptance
Everyone is entitled to their own personal religious beliefs. We live in a world where there are religions and beliefs that see LGBT people as negative and there are those who embrace LGBT people with open arms. We are so sorry if someone has ever used religion or their faith to make you feel little, worthless or bad for who you are.
There are many religions in the world, with varying degrees of acceptance of the LGBT community. Often times, though, it comes down to individual congregations. There are welcoming, accepting congregations within most religions, and if you have specific questions or would like to be involved with any particular one, we’re more than happy to look for a local resource for you to explore that more with that community near you, or for some organizations within that religion that exist to support LGBT people on a national scale.
It is important to understand that each person is free to follow their own beliefs and faith. A person does not need to follow the doctrines or faith of anyone else’s religions even if it is their parents or family’s. Your faith is yours and yours alone.
There are more and more people of every religion that are coming to understand that a person’s sexuality and/or gender identity has nothing to with their ability to be people of faith. A person’s sexuality and/or gender identity does not determine if they are a good or bad person.
Can you talk to me about what the Bible/other texts say? -We can’t.
Religious text from any religion can be seen as historical documents and a product of a certain time and place. Many religious texts have been translated or edited over several thousands of years by different sects and congregations, so there can be many different viewpoints.
We aren’t capable of getting into the specifics of what any given religion believes or to debate any texts or passages which speak about LGBT-related topics.
We’re not trained to get into debates about various passages or text in the Bible, the Torah, the Quran or other religious texts. The LGBT Help Center isn’t associated with any religion, and we can’t share any personal beliefs.
If you have questions about religion and specifics, we can see if we can find LGBT affirming congregations or churches near you that you can have those discussions with.
Trust your instincts
Assess if caller is willing to focus on feelings
Do not engage, scold or argue
Examine caller history
Don't ASK if you've spoken before, just STATE it
Focus call on recent time frame
Be assertive "breaking in"
Steer back to "FOCUS"
Call it out
Closed-ended questions
Reassure call is anonymous and confidential
Give positive reinforcement
Be silent
Call it out
Open-ended questions
Two minute warning
Call it out
Closed-ended questions
Mandated Reporting
It’s important to remember that the LGBT National Help Center is not a mandated reporter. Even if you are a mandated reporter in your job, while volunteering with us, you are not.
What is a “mandated reporter?”
A mandated reporter is someone who is required to report specific situations to the appropriate authorities. Many hotlines act as mandated reporters, meaning that if a caller is in an emergency, they have the ability to contact 911, medical assistance, or other emergency-related services. We are not mandated reporters. That means that we cannot, under any circumstances, contact emergency services (or anyone else) on a caller’s behalf. This is an extremely strict policy that we have to follow, because of the potential legal liability of becoming responsible for something that we are not equipped to handle.
We have made a promise to our callers that our calls are anonymous and confidential and reporting would be breaking that promise which could lead to them never trusting us or other services again.
As a volunteer, you will never make any phone calls or become involved in any way during a caller’s emergency even if the caller asks.
POSSIBLE SCRIPT: I’m sorry, we can’t make an outgoing call on your behalf, but I can see if I can find the appropriate number for you to call with.
There are a few times (very very rare), when you may need to contact Aaron to proceed in taking action. If there is a caller who has stated a threat of violence or terrorism (either has already carried out or in the future) against other people (not the caller themselves). In this situation text Aaron (his number is on the CONTACT page) if you do not get a reply, please call him at the same number. If for some reason you can't get through to him please call the office next at 414-355-0003 and leave as detailed as possible message. (when the call came in, which hotline, what was the threat, any location or identifying information)
He will make the final decision on how to proceed, you will not be asked to make any out going-calls.
(this information can also be found in the INFO CENTER)
For callers in their teens or early 20's: Trevor Helpline (24/7):
Toll-free: 1-866-488-7386
(numbers below are not LGBT specific but affirming)
For callers older than early 20's: 1-800-SUICIDE (1-800-784-2433) OR 988 (call or text available)
Online chat: www.suicidepreventionlifeline.org/chat
CANADA ONLY: 833-456-4566
Conversations rarely work like a flow chart, you can use the pieces of the assessment model that works the best for the individual conversation.
You say: "I'm hearing you say (describe the self-destructive behaviors, signs of suicide you are hearing). Are things so bad that you are thinking about suicide?" (use the word SUICIDE).
If the caller answers NO, you say: "I'm glad to hear you say that. But if you were, we could definitely talk about that."
IF THE CALLER ANSWERS YES, use whichever questions are needed (you don’t have to use all 5) and talk about each one before moving on to the next.
Do you have a plan?
Do you have the means?
Have you set a time?
Have you attempted suicide before?
Have you done something to hurt yourself now?
The more "yes" answers you receive,
the higher the degree of suicide risk.
After working through the model:
ASK OPEN-ENDED QUESTIONS: "Tell me what you are feeling that is making you feel like committing suicide."
STEER TOWARDS THE PAIN: The caller frequently cannot or will not talk to anyone else about their strongest emotions.
AFFIRM THE CALLER'S FEELINGS: "It really makes me sad to hear that you are in so much pain. This must be very difficult for you.
Remember, the goal is to defuse the intensity of the caller's feelings, to give them a chance to vent and be heard. You can't put their life back together for them -- and you can't save their lives for them either. You don't have that kind of power!
When possible use near future-focused language. It can help diffuse suicidal feelings for the present moment and allow a caller to have an opportunity to plan their next move, without suicide. Focus primarily on the near future specifically, as it can be too stressful for most suicidal callers to focus on things too far in advance.
“Can you think of something that might help you get through the next hour?”
“What’s something that has helped you in the past when you have felt (Suicidal/anxious/depressed/overwhelmed/etc.)?
“Can you think of something that you might be able to do tomorrow?”
“Would you like to brainstorm some things with me that you can do once we’re off the phone?”
IF CALLER FINDS IT DIFFICULT TO THINK OF THINGS TO DO NOW/LATER:
“If you’d like to, you can take a couple of minutes to just breathe – I’ll stay on the line so when you feel ready to talk. Take your time.”
Safety Plan can be found in the INFO Center and found on site, lgbthotline.org under RESOURCES
SELF-HARM info can be found in the INFO CENTER in its own button and can be found on our website www.lgbthotilne.org under RESOURCES.
Some people cut or self-harm to try to cope with pain or strong emotions, intense pressure or upsetting problems. It may be a way for them to feel control in a situation they feel helpless in. It can be a way to express pain they can’t put into words. It can be a way to feel something (even if it’s pain) at a time they are having trouble being able to feel anything at all.
The relief that comes from self harm does not last long. It can quickly be followed by feelings like guilt or shame. It can become addictive. It’s possible to hurt ones self badly.
Finding coping techniques or finding other outlets can help in times a person feels the need to cut.
Below are lists of ideas to focus on instead of self-harming.
Start a journal/blog/vlog
Write a story or poetry
Compose music
Paint/draw/color
Play a musical instrument
Scribble on paper
Create something in clay
Sing
Talk to yourself
Build/Craft something
Exercise
Punch a pillow
Throw socks
Use a stress ball
Make noise/scream as loud as you can (in a safe or private space)
Squeeze clay
Stomp your boots
Instead of cutting, cover yourself in band-aids
Write the names of special people or thoughts on your arms
Tear up an old newspaper
Draw slash lines on paper
Take a warm shower or bath
Pet or cuddle a dog or cat
Wrap yourself in a blanket
Message your neck, hands, or feet
Listen to calming music
Hug a pillow or stuffed animal
Paint your nails
Watch a favorite movie
Re-read a favorite book
Go for a nice walk
People watch
Count ceiling tiles or lights
Meditate
Talk to friends
Take a COLD shower
Hold ice in the crook of your leg or arm
Chew something strong like chili, lemon, or peppermint
Snap a rubber band on you wrist for brief periods of time
Focus deeply on a piece of chocolate as you eat
Blow up a balloon and pop it
Connect online with help forums
Concentrate on things that have made you happy in the past
Perform 1 act of kindness
Volunteer somewhere
Pay someone a compliment
Pay it forward
Do you feel safe in that situation?
Was that something that you felt comfortable doing?
Do you feel like you had a choice in that situation?
Did you feel like you had control over what happened?
IT IS NOT YOUR FAULT
You deserve to be treated with respect and kindness
I’m sorry that someone made that decision for you
Consent is absolutely necessary, and it means that everyone involved has to be in full agreement of what is happening. Any person involved at any time can take back their consent.
Do they sound like they had a choice in the situation? If unsure, ask.
Do they sound uncomfortable? If so, explore why.
Is the caller a minor? If so, are they talking about sexual contact with someone who is over the age of consent? (If this is the case, point out that it is illegal)
Is the caller an adult discussing sexual contact with a minor? (if this is the case, point out that it is illegal)
If the caller has sexually assaulted another person. We can let them know there may be legal ramifications for their actions, however we can not continue the conversation with them. There may be a lot they would like to discuss and they would be better served by talking with a professional counselor or therapist. We can do a research search for them for continued aid.
Additional help beyond us:
RAINN (800-656-4673)
Police (if they choose – however, this is not always an option or something they want to do. If someone is nervous about contacting police/making a report, they can call the local non-emergency number for the police station and ask anonymous questions)
If it is a minor, they can contact the Child Abuse Line (If they have a private phone, they can ask if the line is a mandated reporter and what that can mean for their privacy)
If it is a person in a relationship with the perpetrator, they can contact the National Domestic Abuse Hotline, RAINN.
We have seen a rise in calls from callers who identify as asexual. Asexuals (Aces) can identify themselves as part of the LGBTQIA community. Some may not identify as part of a larger community. Both identities are valid.
Asexuality can be used as an umbrella term to include asexual, aromantic, gray-ace and many other identities. Asexuality is varied and can be different for each individual. There is no one-way of being asexual as each person’s experience is different. The connection can be a general sense of having no (or low) sexual attraction or desire for sexual activity.
Some people use the term Asexual to define their sexual orientation, as they may not identify as gay, lesbian, straight, bisexual or pansexual and have no desires for other individuals.
Some people use Asexual in addition to their sexual identity (example, gay and asexual or homoromantic) who may have no desire for sexual activities but do have romantic or physical attraction towards others.
An Asexual person can be asexual and gay, lesbian, straight, bi or pan.
An Asexual person can also identify as cisgender or transgender, their asexuality is not connected to their gender identity.
A person can have sex and still identify as asexual, it is more focused on their attractions and desires.
Ace – Short or slang for Asexual.
Aromantic: An Aromantic (aro for short) person is one who experiences little or no romantic attraction to others. It is possible for an aromantic person be involved in and enjoy a devoted relationship with another person, but those relations may be closer to friendship and not a romantic one.
Bi/pan-romantic asexual: A person who is romantically attracted to more than one gender, but does not necessarily have sexual attractions.
Gray –a / gray ace: A person who falls between being asexual and sexual.
Gray-romantic: A person with a romantic orientation that is somewhere between aromantic and romantic.
Heteroromantic asexual: A person who is romantically attracted to a member of the another gender, but does not necessarily have sexual attractions.
Homoromantic asexual: A person who is romantically attracted to a member of the same gender, but does not necessarily have sexual attractions.
(LGBT people experiences around the world are different; some are much harder living in counties where it may be illegal to be LGBT. We are receiving more and more inquires about immigration from those seeking a safe life. We’re not lawyers so we can’t give legal advice. We can say that seeking entrance into the US has become very difficult with laws changing quickly. Below are some general aids for those seeking immigration support. If possible it is advisable to seek legal aid when moving to a new country, as there are many rules and regulations.
Resources can be found in the database under Legal: Immigration
Asylum : Asylum is a protection granted to foreign nationals already in the United States or at the border who meet the international law definition of a “refugee”.
A Refugee is a person who is unable or unwilling to return to their home country and cannot obtain protection from that country, due to past persecution or a well-founded fear of being persecuted in the future on the account of race, religion, nationality, or membership in a particular social group or political opinion.
For more information on Asylum seeking: www.USCIS.gov/Humanitarian
Immigration: Foreign citizens who want to live permanently in the US must first obtain an immigration visa. It is a complex process. It is highly encouraged to seek legal counsel.
Federal website for information on immigration: www.travel.state.gov
Nonimmigrant Visas: An endorsement on a passport indicating that the holder is allowed to enter, leave or stay a specific period of time in a country. There are different type of visas, tourist/visitor, work and student being most common. These are ways to be able to come to a country legally for a specific amount of time. One may be able to seek asylum as a visa holder, though talking with a legal advisor is highly advisable.
Student Visa (a type of Nonimmigrant visa)
It’s important to know that before you can apply for a student visa, you must first apply and be accepted by a US institution of higher learning that is certified by the Student Exchange and Visitor Program (SEVP). For more information you will need to contact the school you are interested in enrolling in.
Work and Tourist/visitor visas have many different requirements and rules and can be explained on the US travel information website.
For information on Nonimmigrant Visas: www.travel.state.gov and look under US Visas
*Note , there are other countries that are more welcoming than the US, such as Canada or Australia. Due to the Safe Third Country Agreement, asylum seekers can not go through the US to seek asylum in Canada. (AS OF OCT 2020)
Canadian immigration/asylum info: www.canada.ca/en/services/immigration-citizenship.html
Australia immigration/asylum info: : www.australia.gov.au, then search Immigration and Visas